What is Malaria?
Malaria is a life-threatening disease caused by Plasmodium parasites, which are transmitted to humans through the bites of infected female Anopheles mosquitoes. Despite being preventable and treatable, malaria remains a major global health issue, especially in tropical and subtropical regions.
This disease poses a significant threat to public health, with millions of cases reported annually. Its effects range from mild symptoms like fever to severe complications that can lead to death. Understanding malaria is essential to combating its spread and ensuring early intervention.
Causes and Transmission of Malaria
Malaria is primarily caused by five types of Plasmodium parasites:
- Plasmodium falciparum – The most common and deadliest.
- Plasmodium vivax – Known for causing recurring infections.
- Plasmodium ovale – Rare, but can cause prolonged illness.
- Plasmodium malariae – Known for chronic infections.
- Plasmodium knowlesi – A zoonotic species found in Southeast Asia.
How is Malaria Transmitted?
- Mosquito Bites: The Anopheles mosquito is the primary carrier, injecting parasites into the bloodstream when it bites.
- Blood Transfusion: Rarely, malaria spreads through transfused blood from an infected individual.
- Mother to Child: Infected mothers can pass the parasite to their unborn babies during pregnancy (congenital malaria).
- Shared Needles: In rare cases, sharing needles contaminated with infected blood can cause transmission.
Key Risk Factors
You are at a higher risk if you:
- Live in or travel to regions with high malaria prevalence.
- Lack access to preventative measures like mosquito nets or repellents.
- Have a compromised immune system, such as young children or pregnant women.
Understanding these factors helps in implementing preventive strategies effectively.
Symptoms of Malaria
Malaria symptoms typically appear within 10 to 15 days of being bitten, but some cases can take months to manifest, depending on the parasite type.
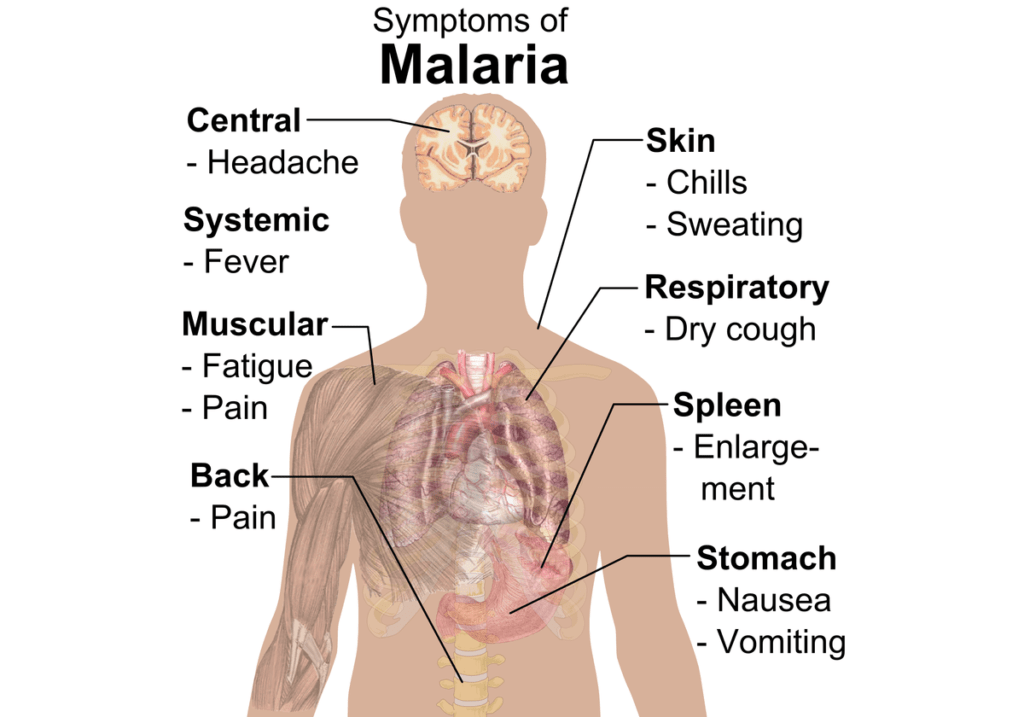
Common Symptoms
- Fever
- Chills and Sweats
- Headache
- Muscle Pain
- Fatigue
- Nausea and Vomiting
Severe Malaria Symptoms
- Confusion or altered mental state.
- Severe anemia.
- Difficulty breathing, Dry Cough.
- Organ failure (e.g., kidneys or liver).
The Symptom Cycle
Malaria is infamous for its cyclical nature. Patients often experience:
- Cold Stage: Intense shivering.
- Hot Stage: High fever and rapid heartbeat.
- Sweating Stage: Profuse sweating as the fever breaks.
These stages often recur every 2–3 days, depending on the parasite.
Prevention of Malaria
Prevention is the most powerful weapon against malaria. Here’s how you can reduce your risk:

1. Use Mosquito Nets
Sleeping under insecticide-treated mosquito nets (ITNs) is one of the most effective preventive measures, especially in high-risk areas.
2. Apply Mosquito Repellents
- Choose repellents with DEET, picaridin, or lemon eucalyptus oil.
- Apply on exposed skin and clothing.
3. Eliminate Breeding Grounds
- Remove stagnant water from containers, drains, and puddles.
- Maintain a clean and dry environment around your home.
4. Preventive Medications
- Antimalarial Drugs: Consult a doctor for prophylactic medications like doxycycline or mefloquine if traveling to malaria-prone areas.
5. Protective Clothing
Wear light-colored, long-sleeved shirts and pants to minimize mosquito bites.
6. Vaccination
While vaccines like RTS,S/AS01 (Mosquirix) have shown promise, their availability and effectiveness are still limited.
Implementing these measures can significantly lower your chances of contracting malaria.
Diagnosing Malaria
Accurate diagnosis is vital for effective treatment.
When to Seek Testing?
- If you experience fever and have visited a malaria-prone region.
- For symptoms persisting despite other treatments.
Diagnostic Tests
- Microscopic Examination: A blood smear identifies the presence of parasites.
- Rapid Diagnostic Tests (RDTs): These tests detect malaria antigens in a few minutes.
- Polymerase Chain Reaction (PCR): Used for detailed and sensitive identification of malaria strains.
Importance of Timely Diagnosis
Delays in diagnosis can lead to severe complications, making early testing crucial, especially for travelers and residents in high-risk areas.
Treatment of Malaria
Treating malaria promptly and effectively is crucial to avoid severe complications. The choice of treatment depends on factors such as the type of Plasmodium parasite, the severity of symptoms, and the patient’s health condition.

1. First-Line Treatments
- Artemisinin-Based Combination Therapies (ACTs): These are the most common and effective drugs for treating uncomplicated malaria caused by Plasmodium falciparum. ACTs combine artemisinin with another medication to reduce resistance risks.
- Chloroquine: Used for treating P. vivax and P. malariae infections, but resistance is increasingly common.
2. Treatment for Severe Malaria
Severe malaria cases require immediate hospitalization and intravenous treatment. Common options include:
- Intravenous Artesunate: Administered to quickly reduce the parasite load.
- Supportive Care: Includes fluids, oxygen, and blood transfusions if needed.
3. Treating Relapsing Malaria
Relapsing forms like P. vivax and P. ovale need additional drugs like primaquine or tafenoquine to eliminate dormant parasites in the liver.
4. Pregnancy-Specific Treatments
Pregnant women require special care, as malaria can lead to complications such as preterm delivery and low birth weight. Safe options include quinine and clindamycin, depending on the trimester.
Medication Adherence
It’s crucial to complete the full course of antimalarial medication, even if symptoms improve, to prevent recurrence and resistance.
Complications of Malaria
If untreated or improperly managed, malaria can escalate to severe health complications. Understanding these risks underscores the importance of prompt action.
1. Cerebral Malaria: This severe form affects the brain, leading to confusion, seizures, and even coma. It is primarily caused by P. falciparum.
2. Severe Anemia: Parasites destroy red blood cells, leading to dangerously low hemoglobin levels. This is particularly risky for children and pregnant women.
3. Organ Failure: Malaria can result in failure of vital organs like the kidneys, liver, or spleen. Acute respiratory distress syndrome (ARDS) is also a concern.
4. Hypoglycemia: Certain malaria drugs, such as quinine, can cause dangerously low blood sugar levels, especially in children and pregnant women.
5. Maternal and Neonatal Complications: Malaria during pregnancy increases the risk of miscarriage, stillbirth, and neonatal mortality.
Recognizing the signs of severe malaria—like persistent vomiting, convulsions, or breathing difficulties—can save lives.
When to See a Doctor?
It is vital to seek medical attention immediately if you suspect malaria, especially in the following scenarios:
High-Risk Symptoms
- Fever, chills, and severe headache after traveling to or residing in a malaria-endemic area.
- Symptoms persist despite basic fever treatments.
Severe Symptoms
- Seizures, confusion, or loss of consciousness.
- Severe abdominal pain or difficulty breathing.
Pregnancy and Malaria
Expectant mothers experiencing any malaria symptoms should consult a doctor urgently, as the disease can endanger both mother and baby.
Travel Advisory
Travelers returning from malaria-prone regions should monitor their health and consult a doctor at the first sign of fever.
Early medical intervention can make a significant difference in outcomes, reducing complications and fatalities.
Global Impact of Malaria
Malaria continues to be a global health challenge, especially in regions with limited access to healthcare resources.
1. Statistics
- In 2022, the WHO estimated 249 million cases of malaria worldwide.
- 619,000 deaths were attributed to malaria, with the majority occurring in sub-Saharan Africa.
2. Vulnerable Populations
- Children Under 5: Account for over 70% of malaria deaths globally.
- Pregnant Women: At higher risk of severe illness and complications.
3. Economic Burden
Malaria not only impacts health but also imposes a significant economic burden on families, healthcare systems, and national economies.
4. Progress and Challenges
Efforts like insecticide-treated nets and ACTs have reduced malaria cases in some areas. However, challenges such as drug resistance, insecticide resistance, and climate change continue to hinder eradication.
Focusing on preventive measures and improving access to treatments can help mitigate the global impact of malaria.
The Future of Malaria Control and Eradication
Advancements in technology, medicine, and public health strategies offer hope for a malaria-free future.
1. Innovative Vaccines
- The RTS,S vaccine, approved for children in some regions, marks a milestone in malaria prevention.
- Research is ongoing to develop more effective vaccines with broader coverage.
2. Gene Drives in Mosquito Control
Genetic engineering techniques aim to reduce the mosquito population or render them incapable of transmitting malaria.
3. Enhanced Diagnostics
Rapid advancements in diagnostic tools, such as AI-integrated systems, are improving early detection and treatment.
4. Community Engagement
Educating communities about malaria prevention and treatment is crucial for sustainable progress.
By addressing challenges like funding gaps and healthcare inequalities, global malaria eradication could become a reality within the next few decades.
FAQs About Malaria
1. What is malaria?
Malaria is a disease caused by Plasmodium parasites, transmitted through infected mosquito bites.
2. How is malaria diagnosed?
It’s diagnosed through blood tests, including microscopic examination and rapid diagnostic tests (RDTs).
3. What are the first symptoms of malaria?
Common early symptoms include fever, chills, and headache.
4. Can malaria be cured?
Yes, malaria is curable with timely and appropriate treatment.
5. Who is most at risk?
Children under 5, pregnant women, and travelers to endemic areas are at high risk.
6. How does malaria affect pregnancy?
It increases risks like miscarriage, stillbirth, and low birth weight.
7. Is there a vaccine for malaria?
The RTS,S vaccine is available in some regions but has limited coverage.
8. Can malaria return after treatment?
Yes, P. vivax and P. ovale can cause relapses due to dormant liver parasites.
9. What is severe malaria?
Severe malaria involves complications like cerebral malaria, organ failure, or severe anemia.
10. Are there natural remedies for malaria?
No, malaria requires proper medical treatment. Natural remedies may alleviate symptoms but don’t cure the disease.
11. Can I prevent malaria while traveling?
Yes, by taking antimalarial drugs, using insect repellents, and sleeping under mosquito nets.
12. How does malaria affect children?
It can cause severe complications like brain damage or death if untreated.
13. Can animals get malaria?
Yes, some animals can get malaria caused by different Plasmodium species.
14. How do I know if my fever is malaria?
If you’ve been in a malaria-endemic area, consult a doctor immediately for testing.
15. What is the malaria incubation period?
It ranges from 7 to 30 days, depending on the parasite type.
16. Can I donate blood after malaria?
There is usually a deferral period (e.g., 3 years) before donating blood after a malaria infection.
17. Why is malaria common in tropical regions?
Warm climates and stagnant water create ideal conditions for mosquito breeding.
18. How is malaria different from dengue?
While both are mosquito-borne diseases, malaria is caused by parasites, and dengue is caused by a virus.
19. Is malaria contagious?
No, malaria cannot be spread directly from person to person.
20. What are the best preventive measures?
Using insecticide-treated nets, repellents, and taking antimalarial medication are the most effective methods.
Conclusion
Found this helpful? Share this article with your friends and family!

1 thought on “Malaria: How to Spot, Treat, and Prevent This Deadly Disease”