- Introduction
- 1. Overview of Japanese Encephalitis (JE)
- 2. What Causes Japanese Encephalitis?
- 3. How JE Spreads: The Role of Mosquitoes
- 4. Epidemiology: Where is JE Most Prevalent?
- 5. Who is at Risk of Contracting JE?
- 6. Common Symptoms of Japanese Encephalitis
- 7. Stages of JE Infection
- 8. How Japanese Encephalitis is Diagnosed
- 9. Key Tests for Identifying JE
- 10. Understanding the Results: JE Indicators
- 11. Is There a Cure for JE?
- 12. Common Treatment Approaches and Management
- 13. Rehabilitation and Recovery from JE
- 14. Long-Term Health Implications of JE
- 15. Vaccination for JE: Who Should Get It?
- 16. Types of JE Vaccines Available
- 17. Importance of Mosquito Control in Preventing JE
- 18. Travel Precautions for Japanese Encephalitis
- 19. Living with Japanese Encephalitis: Coping Strategies
- 20. Support Networks and Resources for JE Patients
- 21. When to See a Doctor
- FAQs on Japanese Encephalitis (JE)
Introduction
Japanese Encephalitis (JE) is a serious viral infection primarily affecting the brain, transmitted to humans through mosquito bites, specifically by Culex species. Common in parts of Asia and the Western Pacific, this disease often peaks during the monsoon season, where stagnant water provides breeding grounds for mosquitoes. Japanese Encephalitis can lead to neurological damage, including inflammation of the brain (encephalitis), which can result in severe and sometimes fatal health outcomes.
1. Overview of Japanese Encephalitis (JE)
Japanese Encephalitis, commonly referred to as JE, is part of the Flavivirus group, which includes other mosquito-borne viruses like Dengue and West Nile Virus. Although many infected individuals remain asymptomatic, those who do show symptoms can experience mild to severe effects, ranging from fever and headache to seizures, coma, and even death in severe cases. JE is particularly dangerous in rural agricultural areas, where mosquitoes thrive in rice paddies and other wet environments.
Understanding JE’s transmission, impact, and prevention strategies is essential, especially for individuals in or traveling to regions where JE is common. Japanese Encephalitis poses a significant risk to children and older adults, who often experience more severe symptoms when infected.
2. What Causes Japanese Encephalitis?
Japanese Encephalitis is caused by the Japanese Encephalitis Virus (JEV), which is transmitted primarily by infected mosquitoes. The virus naturally exists within an animal reservoir, typically involving birds and pigs. Mosquitoes become infected by biting an infected host and, in turn, can transmit the virus to humans through their bite.
While the virus is not transmissible from human to human, a mosquito biting an infected human could potentially spread the virus to another host. Pigs and birds serve as key amplifiers for the virus, allowing the disease to persist in rural and agricultural regions. These animals are often the main reservoirs for the virus, meaning they carry the virus without suffering significant symptoms but can still pass it to mosquitoes and, indirectly, to humans.
3. How JE Spreads: The Role of Mosquitoes
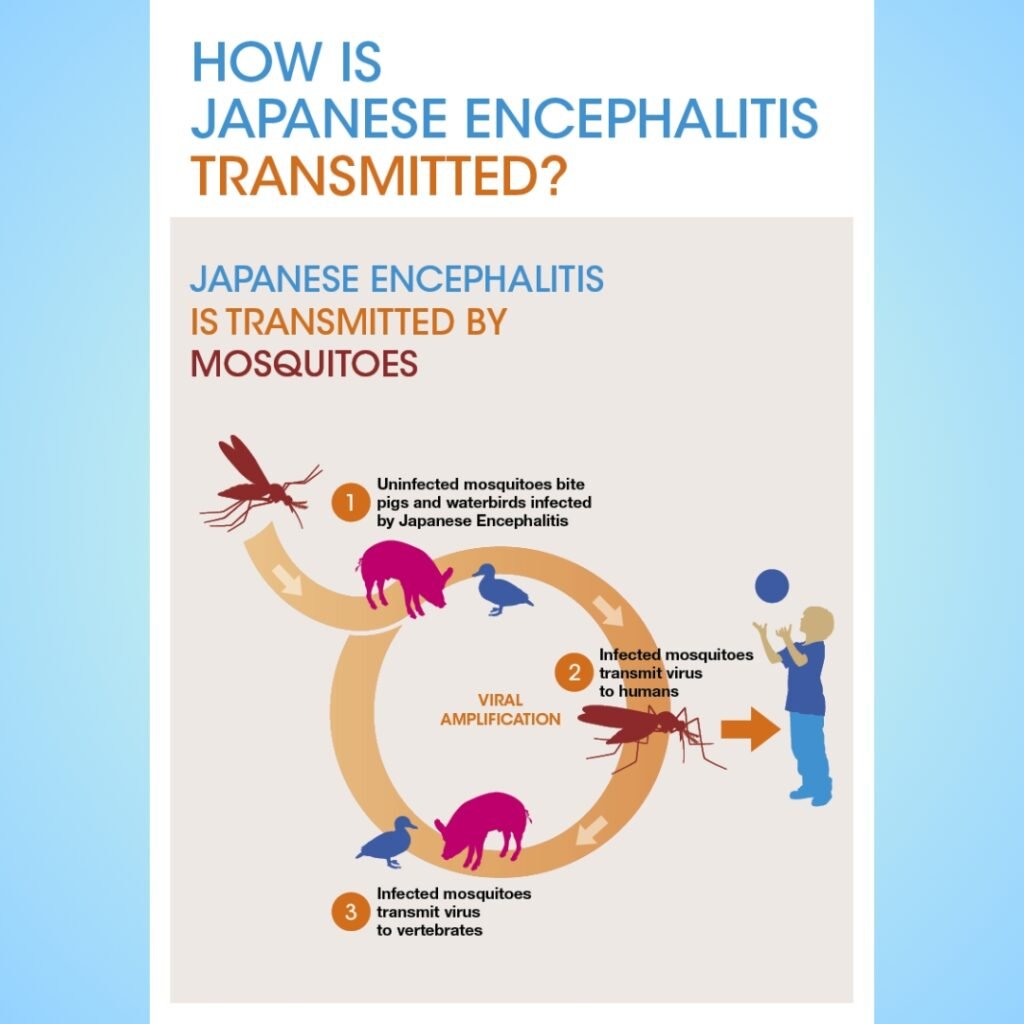
Under Google’s Creative Commons licenses
The spread of Japanese Encephalitis relies heavily on the Culex species of mosquitoes, which breed in standing water and thrive in humid, rural settings. Rice fields, swamps, and marshes offer ideal habitats for these mosquitoes. As a result, Japanese Encephalitis outbreaks often correlate with monsoon seasons and periods of high rainfall when mosquito populations spike.
Mosquitoes contract the JE virus by feeding on infected birds or pigs and then carry the virus in their saliva, ready to transmit it to humans during the next bite. Although JE transmission primarily occurs in rural settings, urban areas with poor sanitation and stagnant water can also experience outbreaks. Travelers visiting endemic regions during mosquito season should take extra precautions to prevent mosquito bites, as the virus can cause severe health issues upon infection.
4. Epidemiology: Where is JE Most Prevalent?
Japanese Encephalitis is found predominantly in parts of Asia and the Western Pacific, where warm, humid climates allow mosquitoes to thrive. High-risk areas include countries like Japan, China, India, Nepal, and Southeast Asian countries, where the virus is endemic. Over three billion people live in regions where JE is prevalent, making it a significant public health concern.
The disease is seasonal in most areas, with increased cases during the rainy season when mosquito populations are at their peak. In countries like Japan and South Korea, extensive vaccination programs have greatly reduced the incidence of JE, but many developing regions still face regular outbreaks due to limited access to vaccines and effective mosquito control.
5. Who is at Risk of Contracting JE?
Japanese Encephalitis affects both locals and travelers in endemic regions, but certain groups are more susceptible to the virus. Children under the age of 15 and the elderly are particularly at risk due to their potentially weaker immune responses. Agricultural workers, such as rice farmers and livestock handlers, also face higher risks as they are frequently exposed to mosquito-prone environments.
Travelers who plan to spend significant time in rural areas, especially in regions with known JE cases, should be vigilant. Backpackers, adventure travelers, and those visiting villages or rural farms may have increased exposure. People with existing health conditions, compromised immune systems, or those who are not vaccinated face a higher likelihood of severe infection if they contract JE.
6. Common Symptoms of Japanese Encephalitis
One of the challenges with Japanese Encephalitis is that most infected individuals—about 99%—do not exhibit symptoms or may experience only mild, flu-like symptoms. However, in cases where symptoms do appear, they often progress rapidly and can be severe.
Early Symptoms:
- Fever: Often the first sign of JE infection.
- Headache: Persistent headaches may accompany the fever.
- Fatigue and Muscle Pain: Weakness and soreness are common.
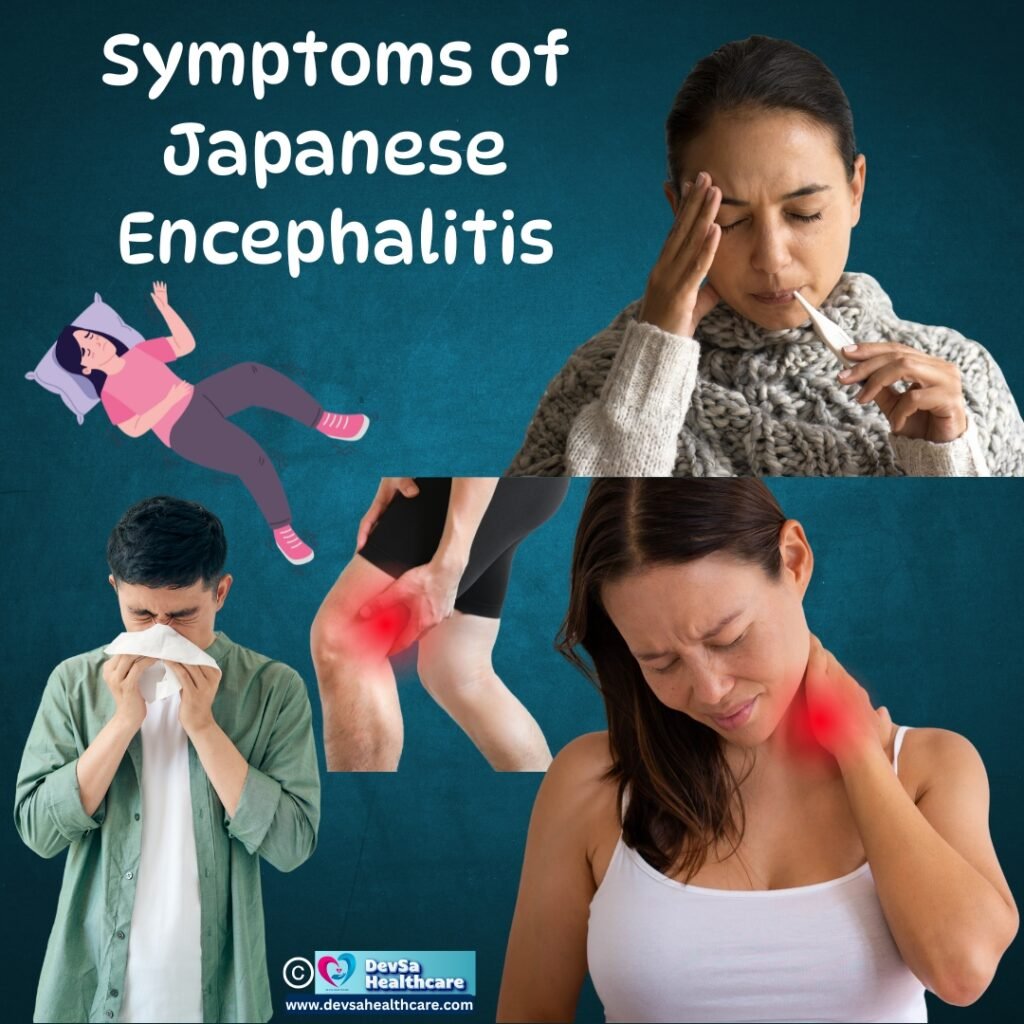
In severe cases, these initial symptoms can progress to neurological symptoms, marking the onset of encephalitis or brain inflammation.
Severe Symptoms:
- Seizures: Convulsions can occur, especially in children.
- Stiff Neck: An indicator of inflammation affecting the brain and spinal cord.
- Altered Mental State: Confusion, irritability, and lethargy may arise as the brain becomes inflamed.
- Tremors and Paralysis: In some cases, paralysis or movement disorders can develop.
As the disease progresses, symptoms can lead to complications like coma and respiratory failure, making early detection critical. Only supportive treatments are available, and without timely intervention, mortality rates for severe JE cases are high.
7. Stages of JE Infection
The Japanese Encephalitis infection follows a distinct pattern, progressing through several stages if the immune system fails to clear the virus early on. These stages illustrate how JE symptoms develop from mild to potentially life-threatening:
- Incubation Period: After being bitten by an infected mosquito, the virus incubates for approximately 5–15 days. During this time, the virus multiplies without causing symptoms.
- Prodromal Stage: Mild symptoms such as fever, fatigue, and headache begin to appear. This stage can last for several days and is often mistaken for other viral infections.
- Acute Encephalitic Stage: The virus reaches the central nervous system, causing severe neurological symptoms. The patient may experience seizures, confusion, and even loss of consciousness. In this stage, the immune system responds aggressively, leading to inflammation in the brain.
- Recovery Stage: If the patient survives the acute stage, recovery begins. However, some individuals may experience neurological impairments for months or years, as JE can cause lasting damage to the brain.
- Long-Term Sequelae: Up to 30% of survivors suffer from permanent disabilities, including cognitive deficits, motor impairments, and emotional disturbances. Supportive therapies can help with recovery, but the effects of JE can be lifelong.
8. How Japanese Encephalitis is Diagnosed
Diagnosing Japanese Encephalitis can be challenging due to the non-specific nature of early symptoms, which mimic other viral infections. However, certain diagnostic methods are used to confirm JE, especially when neurological symptoms are present.
- Medical History and Symptom Evaluation: Doctors begin with a thorough review of the patient’s medical history, travel history, and symptoms to assess potential exposure to JE. Those who have recently traveled to or live in JE-endemic areas are considered higher risk.
- Lumbar Puncture (Spinal Tap): This test is commonly performed in suspected encephalitis cases. A sample of cerebrospinal fluid (CSF) is taken from the spine to detect signs of inflammation and the presence of JEV antibodies, indicating a JE infection.
- Blood Tests for JE Antibodies: Blood samples are analyzed for Immunoglobulin M (IgM) antibodies against JEV. High levels of these antibodies are indicative of a JE infection. Specific tests, like ELISA (enzyme-linked immunosorbent assay), are used for accurate detection.
- Neuroimaging (MRI or CT Scan): Brain imaging helps identify inflammation and other signs of encephalitis. While not specific to JE, neuroimaging can reveal changes that support a JE diagnosis when combined with other test results.
Early diagnosis of JE is crucial to managing symptoms effectively, as there is no cure, and supportive treatment can reduce complications.
9. Key Tests for Identifying JE
Confirming a Japanese Encephalitis infection requires specific tests beyond routine diagnostics due to the complexity of the virus. Laboratory tests for JE aim to detect the virus or immune response markers specific to JEV:
- Serological Testing: The most reliable method for diagnosing JE, serology identifies JEV-specific antibodies in blood or cerebrospinal fluid (CSF). The IgM-capture ELISA test is the standard diagnostic test for JE and has a high sensitivity for detecting acute infections.
- Polymerase Chain Reaction (PCR) Tests: Although not routinely used due to limited availability in many regions, PCR testing can directly detect JEV genetic material in blood or CSF. This method is highly accurate but requires specialized laboratory equipment.
- Virus Isolation: In specialized laboratories, JEV can be isolated from clinical specimens. However, this process is time-consuming and mainly used for research rather than routine diagnostics.
Proper diagnostic procedures help confirm JE in suspected cases, enabling healthcare providers to begin supportive care and implement public health measures to prevent further spread.
10. Understanding the Results: JE Indicators
The results from diagnostic tests for Japanese Encephalitis can indicate several important details about the infection:
- Positive IgM Test: High levels of JEV-specific IgM antibodies in blood or CSF confirm a JE infection. Elevated IgM levels generally indicate an active or recent infection, as the body produces these antibodies in response to JEV.
- PCR Confirmation: Positive PCR results indicate the presence of JEV RNA, confirming an active infection. This result helps to rule out other potential causes of encephalitis and supports a specific diagnosis of Japanese Encephalitis.
- Neuroimaging Findings: MRI or CT scans may show inflammation in the thalamus, basal ganglia, and midbrain—regions commonly affected by JE. Although these findings are not definitive for JE alone, they can help reinforce the diagnosis when combined with serological results.
Accurate interpretation of test results is essential for healthcare providers to tailor appropriate supportive care and monitor the patient’s condition.
11. Is There a Cure for JE?
Currently, there is no specific cure for Japanese Encephalitis. As a viral infection, antibiotics are ineffective, and antiviral drugs specifically targeting JE have not yet been developed. Treatment for JE focuses on managing symptoms, reducing complications, and providing supportive care to the patient during the course of the illness.
Due to the severe impact on the brain and nervous system, early diagnosis and intensive care can improve outcomes for patients. Supportive treatment in a hospital setting, where breathing support, hydration, and seizure management are available, plays a critical role in the survival and recovery of JE patients.
The absence of a cure emphasizes the importance of preventive measures, especially in high-risk areas, where vaccination and mosquito control are key strategies for reducing JE infections.
12. Common Treatment Approaches and Management
Managing Japanese Encephalitis involves supportive treatments that address symptoms and reduce the risk of complications:
- Hospitalization: Patients with confirmed JE often require hospitalization, particularly if neurological symptoms are present. Hospitals offer monitoring, specialized care, and immediate access to interventions if symptoms worsen.
- Respiratory Support: Severe JE cases can affect respiratory function, leading to the need for ventilatory support, such as mechanical ventilation, in cases of respiratory failure.
- Anticonvulsants: Seizures are common in JE patients, particularly in children. Medications to control and prevent seizures are essential for stabilizing the patient’s condition.
- Fluid Management: Patients with JE may have altered fluid and electrolyte balance. Proper hydration and electrolyte correction can help prevent dehydration, which can exacerbate neurological symptoms.
- Pain and Fever Management: Analgesics and antipyretics may be used to reduce discomfort and control fever. Fever can elevate inflammation, so reducing body temperature can aid in managing symptoms.
The focus on symptom management and complication prevention highlights the challenges of JE treatment. Patients who survive may require long-term rehabilitative care for neurological recovery.
13. Rehabilitation and Recovery from JE
For those who survive Japanese Encephalitis, recovery can be a long and challenging process. Many patients experience persistent neurological effects that require ongoing rehabilitation:
- Physical Therapy: Physical therapy is crucial for patients who experience motor impairments, such as weakness or paralysis. Therapy focuses on improving muscle strength, coordination, and mobility.
- Occupational Therapy: This form of therapy helps JE survivors adapt to daily activities. It can be particularly valuable for those with cognitive deficits, helping them relearn basic skills or modify tasks to accommodate impairments.
- Speech and Language Therapy: Some JE survivors have speech difficulties or cognitive impairments. Speech therapy can assist with language recovery, communication skills, and cognitive processing.
- Psychological Support: Depression, anxiety, and mood changes are common in JE survivors, especially those with long-term disabilities. Counselling and support groups provide emotional assistance to help patients adjust to life changes following JE.
Approximately 30-50% of JE survivors face lifelong neurological impairments, which can affect daily life, work, and relationships. Supportive care and rehabilitation services are essential for helping survivors improve their quality of life.
14. Long-Term Health Implications of JE
Japanese Encephalitis has profound long-term impacts on survivors, with many facing neurological issues for years or even permanently:
- Cognitive Impairments: Memory problems, attention deficits, and slowed processing can affect daily tasks and occupational capabilities.
- Motor Disabilities: Weakness, tremors, and paralysis, particularly in the limbs, can limit physical mobility and independence.
- Behavioural Changes: Mood swings, aggression, and social withdrawal are common in JE survivors due to the virus’s impact on brain function.
The long-term health implications of JE highlight the virus’s significant toll on individuals and communities. Access to long-term care and mental health support is crucial for helping survivors reintegrate into their lives and regain independence wherever possible.
15. Vaccination for JE: Who Should Get It?

Vaccination is the most effective way to prevent Japanese Encephalitis, particularly for people in or traveling to high-risk areas. Vaccines for JE are recommended for the following groups:
- Travelers to Endemic Regions: Individuals planning to travel to JE-prone areas, especially rural regions during peak mosquito seasons, should consider vaccination.
- Residents of High-Risk Areas: In JE-endemic regions, residents, especially children, are advised to get vaccinated as part of public health programs to curb JE outbreaks.
- Agricultural Workers: Farmers and individuals who work in environments where mosquitoes are prevalent are at higher risk and often encouraged to receive the vaccine.
There are different types of JE vaccines available, each with specific schedules. Most vaccines require two doses, typically given 4-6 weeks apart, to ensure full immunity. For travellers, it’s important to complete the vaccination series well before entering a high-risk area, as this ensures adequate protection against the virus.
16. Types of JE Vaccines Available
Several JE vaccines have been developed and are available in different countries, each with varying recommendations:
- Inactivated Vero Cell-Derived Vaccines (such as IXIARO): This is the most common JE vaccine for travellers and individuals in endemic areas. It is given in two doses, with a booster dose required after one year.
- Live Attenuated Vaccines: Used in some endemic countries, these vaccines offer long-term immunity with a single dose, but their use is limited to certain age groups and settings.
- Recombinant Vaccines: These newer vaccines are derived from genetically engineered viral components and offer effective immunity. They are used in some countries as part of national immunization programs.
Vaccination programs are widely implemented in high-risk areas, and travellers to these regions are advised to consult a healthcare provider to determine which vaccine is most appropriate for their needs.
17. Importance of Mosquito Control in Preventing JE
Since Japanese Encephalitis is spread by mosquitoes, mosquito control is a critical strategy in preventing JE outbreaks. Effective mosquito management can significantly reduce transmission rates, particularly in high-risk regions.
Key mosquito control measures include:
- Eliminating Standing Water: Mosquitoes breed in stagnant water, so removing or treating standing water sources around homes, farms, and villages can help reduce mosquito populations. This includes emptying water containers, covering water storage tanks, and draining puddles.
- Using Mosquito Nets: Sleeping under mosquito nets, especially in rural and high-risk areas, provides protection during the night when mosquitoes are most active.
- Applying Insecticides and Repellents: Insecticides can be sprayed in areas prone to mosquito breeding, while personal mosquito repellents (such as DEET or picaridin) provide an additional layer of protection, especially for travellers and outdoor workers.
- Implementing Community-Based Programs: Community engagement in mosquito control, such as public health education and neighbourhood cleaning efforts, can help reduce the overall risk of JE transmission. Local governments and health agencies often work with communities to raise awareness and encourage participation in mosquito management.
Mosquito control remains a cornerstone of JE prevention, particularly in regions where vaccination coverage is limited.
18. Travel Precautions for Japanese Encephalitis
For travellers visiting JE-endemic areas, especially rural or agricultural regions, taking preventive steps against JE is essential:
- Get Vaccinated: Vaccination is the best preventive measure for travellers who will spend extended time in JE-prone areas. Travelers should receive their JE vaccine doses well before departure to allow time for immunity to build.
- Wear Protective Clothing: Long-sleeved shirts, long pants, and socks can protect against mosquito bites, especially during the evening and night when mosquitoes are most active.
- Use Mosquito Repellents: Applying insect repellent on exposed skin can help prevent bites. Choose repellents with active ingredients like DEET, picaridin, or oil of lemon eucalyptus for effective protection.
- Stay in Screened or Air-Conditioned Accommodation: Staying indoors during peak mosquito hours and choosing accommodations with screened windows or air conditioning reduces exposure to mosquitoes.
- Avoid High-Risk Areas: If possible, avoid rural areas, rice paddies, and other places where mosquitoes are common during peak transmission seasons.
By following these travel precautions, travellers can significantly reduce their risk of contracting JE during their stay in high-risk regions.
19. Living with Japanese Encephalitis: Coping Strategies
For JE survivors, adjusting to life after infection can be challenging, especially for those dealing with long-term neurological impacts. A combination of medical care, lifestyle adjustments, and emotional support is essential for improving quality of life.
- Physical Rehabilitation: Regular physical therapy can help survivors regain strength, mobility, and coordination. Rehabilitation sessions are tailored to the individual’s needs, targeting specific areas affected by the infection.
- Cognitive and Speech Therapy: Patients with cognitive impairments or speech difficulties can benefit from specialized therapy. Cognitive exercises, memory training, and speech therapy can help JE survivors regain cognitive and language skills over time.
- Building a Support Network: Emotional support from family, friends, and healthcare providers is essential for JE survivors. Support groups, either in-person or online, provide a space for individuals to share experiences and receive encouragement from others facing similar challenges.
- Maintaining a Healthy Lifestyle: A balanced diet, regular exercise, and sufficient sleep can help improve mental and physical well-being, aiding in recovery and reducing stress.
Coping with JE’s effects requires patience, resilience, and a comprehensive support system. With consistent rehabilitation and support, many survivors are able to adjust to their new circumstances and live fulfilling lives.
20. Support Networks and Resources for JE Patients
For those affected by Japanese Encephalitis, access to support networks and resources can make a significant difference in the recovery journey:
- National and Local Health Programs: Some countries with high JE prevalence provide support services and rehabilitation programs through their healthcare systems. These programs may include counselling, physical therapy, and access to resources for long-term care.
- Non-Profit Organizations and Charities: Organizations focused on neurological health or mosquito-borne diseases often offer support to JE patients and families. These organizations may provide information, financial aid, and support groups for JE survivors.
- Online Support Groups and Communities: Online communities allow JE survivors and their families to connect with others who have faced similar challenges. Sharing experiences and coping strategies can be incredibly beneficial for mental health and recovery.
- Counselling and Mental Health Services: The psychological impact of JE can be significant, particularly for those dealing with chronic impairments. Counselling services and mental health professionals provide essential support to help survivors manage stress, depression, and anxiety.
Building a strong network of resources enables JE survivors and their families to manage the long-term impacts of the disease and enhances their ability to cope with the challenges they face.
21. When to See a Doctor
Recognizing the signs of Japanese Encephalitis and seeking prompt medical attention can make a critical difference in health outcomes. Knowing when to see a doctor is essential, especially for individuals in high-risk areas or those exhibiting symptoms after mosquito exposure.
Early Symptoms
If you or someone you know begins experiencing symptoms like fever, headache, or fatigue after traveling to or residing in a JE-endemic area, it’s advisable to consult a doctor. While these symptoms are often mild, they could indicate the onset of JE or another viral infection requiring medical evaluation.
Symptoms That Require Immediate Medical Attention
If symptoms progress to severe neurological indicators—such as seizures, confusion, altered consciousness, or a stiff neck—seek emergency medical care immediately. These symptoms suggest encephalitis, which can rapidly progress to life-threatening complications.
Routine Follow-Up Care for JE Patients
For those diagnosed with JE, follow-up appointments and regular check-ups are important to monitor neurological health and assess recovery progress. Healthcare providers may recommend additional tests, therapies, or specialist consultations to manage long-term symptoms and support rehabilitation.
FAQs on Japanese Encephalitis (JE)
Conclusion: Protecting Yourself and Others from Japanese Encephalitis
Found this helpful? Share this article with your friends and family!


1 thought on “Prevent Japanese Encephalitis: 21 Life-changing Facts You Need to Know”