- Overview
- 1. Understanding Epilepsy: What It Is and How It Affects People
- 2. What Causes Epilepsy?
- 3. Types of Epilepsy and Seizures Explained
- 4. Early Signs and Symptoms of Epilepsy to Watch Out For
- 5. How is Epilepsy Diagnosed? Tests and Procedures
- 6. Effective Treatments for Epilepsy
- 7. When to See a Doctor: Red Flags You Shouldn't Ignore
- 8. Living with Epilepsy: Tips for Daily Management
- 9. Impact of Epilepsy on Mental Health
- 10. Epilepsy in Children: Challenges and Solutions
- 11. Epilepsy in Adults and Seniors: Special Considerations
- 12. Myths and Facts about Epilepsy
- 13. Emergency Care for Seizures: What to Do
- 14. Future of Epilepsy Treatment: Ongoing Research and Advances
- 15. When to See a Doctor?
- 16. Frequently Asked Questions (FAQs)
Overview
Epilepsy is a neurological disorder characterized by recurrent seizures, affecting millions worldwide. It can occur in anyone, regardless of age or gender, and the impact varies from person to person. Seizures happen when abnormal electrical activity in the brain disrupts normal function, leading to episodes of unusual behavior, sensations, or sometimes loss of consciousness.
While epilepsy can be managed effectively in most cases, it requires proper understanding, diagnosis, and treatment to ensure patients live a healthy, productive life. This article explores the causes, symptoms, treatments, and when it’s necessary to see a doctor.
1. Understanding Epilepsy: What It Is and How It Affects People
Epilepsy is not a singular disease but a spectrum of disorders with various causes, seizure types, and severity levels. Some individuals experience brief, mild seizures, while others may suffer from more severe convulsions that affect their daily activities.
What Happens During a Seizure?
During a seizure, the brain’s electrical impulses are disturbed, causing abnormal behavior. Depending on the type of seizure, a person may experience involuntary movements, a blank stare, confusion, or uncontrollable jerking movements. Others may simply “zone out” for a few seconds without even realizing they had a seizure.
Epilepsy vs. Other Seizure Disorders: Key Differences
It’s essential to understand that not all seizures indicate epilepsy. Epilepsy involves multiple unprovoked seizures over time, while isolated seizures can be caused by high fever, head injuries, or drug withdrawal. Proper diagnosis ensures the right treatment and distinguishes between epilepsy and other seizure-related conditions.
2. What Causes Epilepsy?
Epilepsy can develop for a variety of reasons, and in some cases, the cause remains unknown. Researchers continue to investigate potential factors, but here are the most common causes:
Genetic Factors
Genetic predisposition plays a significant role in some epilepsy cases. People with a family history of epilepsy may have a higher chance of developing the disorder. Specific gene mutations can alter brain function, making certain individuals more prone to seizures.
Brain Injuries and Trauma
Severe head injuries, including concussions, can damage brain tissue and disrupt normal neural pathways, increasing the likelihood of seizures. Traumatic brain injuries (TBI) from accidents are a common cause of epilepsy, particularly in young adults.
Infections and Brain Disorders
Brain infections like meningitis, encephalitis, or neurocysticercosis can trigger epilepsy by causing inflammation and damage to the brain. Other neurological conditions, such as stroke or brain tumors, are also known to increase the risk of epilepsy later in life.
3. Types of Epilepsy and Seizures Explained
Epilepsy can present in different forms, with seizures varying in intensity and duration. Knowing the types of seizures is essential for effective management and treatment. Doctors generally classify seizures into three major categories based on their origin and behavior:
Focal (Partial) Seizures
Focal seizures start in a specific part of the brain and can affect consciousness or awareness. There are two main types:
- Focal Aware Seizures: The person remains conscious but may experience sudden sensory changes like tingling, flashing lights, or distorted smells.
- Focal Impaired Awareness Seizures: These involve confusion, loss of awareness, or unusual repetitive movements like lip-smacking or hand rubbing.
Generalized Seizures
Generalized seizures affect both sides of the brain and typically result in loss of consciousness. Some common types include:
- Absence Seizures: Also known as petit mal seizures, they cause brief lapses in awareness, often mistaken for daydreaming.
- Tonic-Clonic Seizures: These involve convulsions, muscle stiffening, and jerking movements. They are what most people imagine when thinking of seizures.
- Atonic Seizures: The person suddenly loses muscle control and may collapse.
Unknown Seizures
In some cases, the cause of seizures cannot be identified, and doctors may classify them as unknown seizures. These seizures do not fit into focal or generalized categories but still require treatment.
4. Early Signs and Symptoms of Epilepsy to Watch Out For
Identifying epilepsy early is crucial for prompt treatment. The symptoms can differ depending on the type of seizure, but recognizing warning signs helps individuals seek medical care quickly.
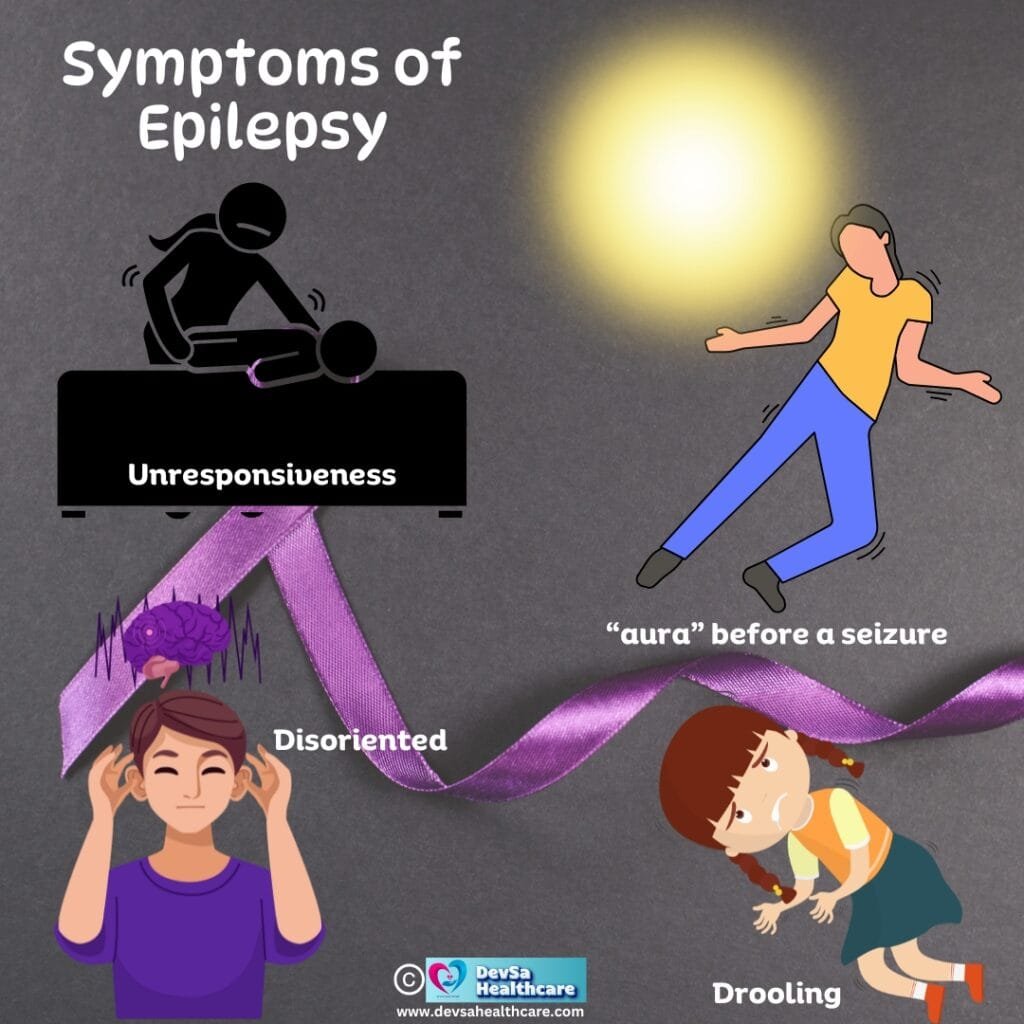
Common Warning Signs Before a Seizure
Some people experience an “aura” before a seizure—a sensation or feeling that acts as a warning. Auras may involve strange smells, tastes, or déjà vu sensations. Others might feel dizziness or unusual emotions, like intense fear.
Physical Symptoms During a Seizure
- Sudden jerking movements (especially of arms and legs)
- Staring spells with unresponsiveness
- Stiffening of the body and loss of muscle control
- Breathing difficulty or drooling
Post-Seizure Recovery Symptoms
After a seizure, individuals often feel disoriented, tired, or confused. Some experience headaches, sore muscles, or temporary memory loss. This recovery phase can last a few minutes to several hours.
5. How is Epilepsy Diagnosed? Tests and Procedures
Diagnosing epilepsy requires careful evaluation by a neurologist, often involving a combination of tests and procedures to confirm the condition.
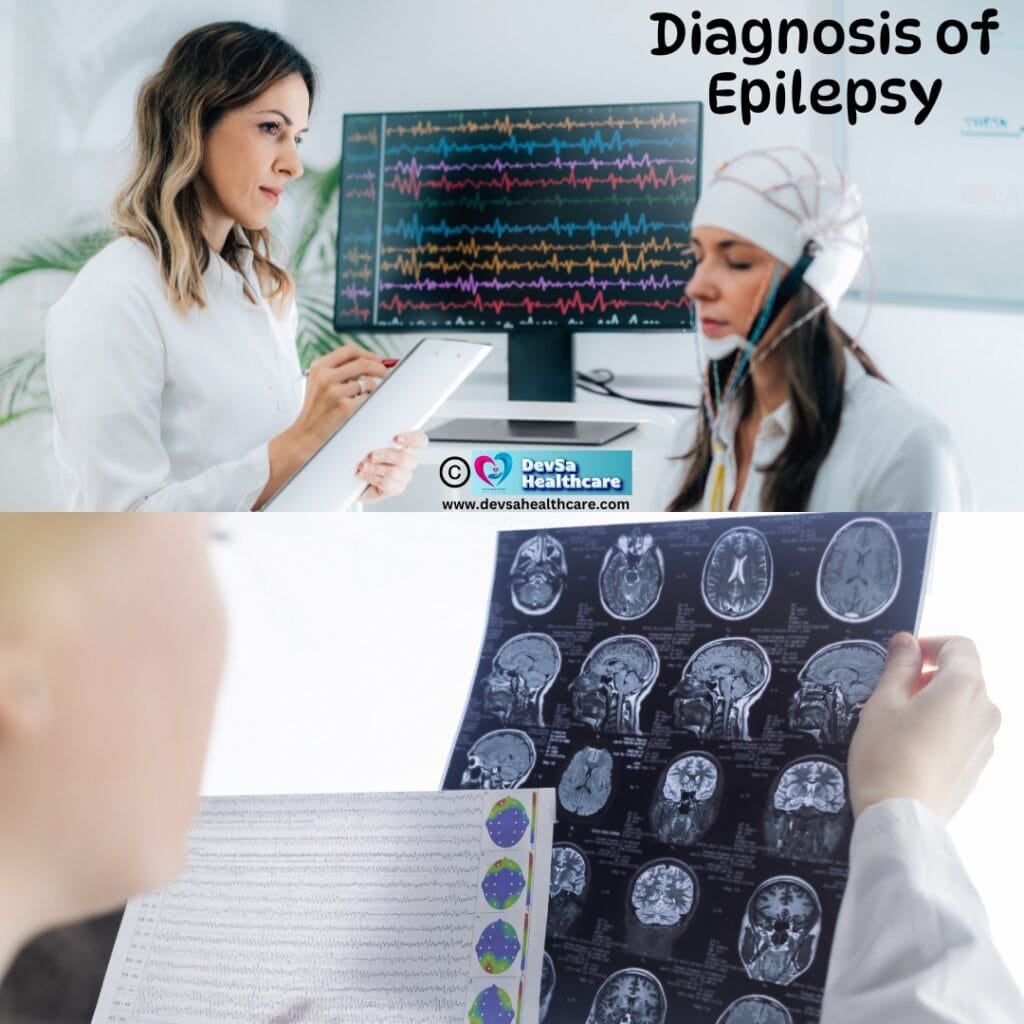
Medical History and Neurological Exams
The first step in diagnosis involves a thorough review of the patient’s medical history and seizure descriptions. Doctors may ask about the duration, triggers, and frequency of seizures, along with any family history of epilepsy. Neurological exams help assess brain function and reflexes.
EEG (Electroencephalogram) Test
An EEG test records the brain’s electrical activity, identifying abnormal patterns that indicate seizures. Patients wear electrodes on their scalp, and the test is painless. Sometimes, doctors may ask patients to sleep or breathe deeply to provoke seizure-like activity during the test.
Brain Imaging: MRI and CT Scans
To rule out underlying brain conditions, doctors may recommend MRI (Magnetic Resonance Imaging) or CT (Computed Tomography) scans. These imaging tools detect structural abnormalities like tumors, scar tissue, or injuries that could trigger seizures.
6. Effective Treatments for Epilepsy
Managing epilepsy often involves a combination of treatments, tailored to the patient’s needs. While some people achieve full seizure control with medication, others may require surgery or alternative therapies. Treatment plans are highly individualized, and finding the right combination may take time.
Anti-Seizure Medications
Anti-seizure drugs (also called anticonvulsants) are the most common form of treatment. These medications help regulate electrical activity in the brain to prevent seizures. Some widely prescribed drugs include carbamazepine, lamotrigine, valproate, and levetiracetam. However, finding the right medication involves trial and error since different drugs work better for different types of epilepsy.
- Side Effects: Fatigue, dizziness, weight changes, and mood swings are common side effects. Close monitoring by a doctor is essential.
Surgery Options for Drug-Resistant Epilepsy
In cases where medication does not provide relief, surgery may be considered. Resective surgery removes the part of the brain causing seizures, while corpus callosotomy interrupts communication between brain hemispheres to prevent seizure spread.
- Success Rate: Surgery offers high success rates, especially for focal seizures that don’t respond to drugs.
Alternative Therapies: Ketogenic Diet, VNS, and CBD Oil
Some individuals explore non-traditional treatments alongside medication:
- Ketogenic Diet: High-fat, low-carb diets have shown effectiveness in children with drug-resistant epilepsy.
- Vagus Nerve Stimulation (VNS): A small device implanted in the chest sends mild electrical pulses to the brain to reduce seizures.
- CBD Oil: Cannabidiol (CBD), derived from cannabis, has shown promise in reducing seizures, especially in severe childhood epilepsy syndromes like Dravet syndrome.
7. When to See a Doctor: Red Flags You Shouldn’t Ignore
While occasional seizures can happen due to various factors, certain signs indicate a need for immediate medical attention. Seeking help at the right time can prevent complications and ensure effective management.
First-Time Seizures
If someone experiences a seizure for the first time, it’s essential to consult a doctor, even if the episode was brief. A neurologist will determine whether the seizure was isolated or the start of epilepsy.
Frequent or Prolonged Seizures
Experiencing multiple seizures within a short time or seizures lasting longer than 5 minutes (status epilepticus) requires urgent medical care. Prolonged seizures can damage the brain and be life-threatening if untreated.
Impact on Mental Health or Daily Activities
If seizures interfere with work, social life, or emotional well-being, a doctor’s intervention is crucial. Mental health challenges such as anxiety or depression often accompany epilepsy, and proper management can improve quality of life.
8. Living with Epilepsy: Tips for Daily Management
Living with epilepsy requires consistent management strategies to maintain a healthy lifestyle and minimize the risk of seizures. With the right care, people with epilepsy can lead fulfilling lives.
Medication Compliance and Routine
Taking medications exactly as prescribed is one of the most important aspects of epilepsy management. Missing doses or stopping medication abruptly can trigger seizures.
- Tip: Set reminders or use a medication management app to stay on track.
Avoiding Triggers and Stress Management
Common seizure triggers include lack of sleep, stress, flashing lights, and alcohol. Identifying personal triggers through a seizure diary helps avoid or minimize exposure to these factors.
- Stress Reduction: Yoga, meditation, and breathing exercises can help manage stress, reducing the frequency of seizures.
Safety Measures at Home and Work
Seizures can occur unexpectedly, so it’s essential to create a safe environment.
- At Home: Remove sharp objects and avoid activities like unsupervised swimming.
- At Work: Inform employers and co-workers about your condition and seizure first aid to ensure prompt assistance if needed.
9. Impact of Epilepsy on Mental Health
Epilepsy affects not just the body but also the mind. Living with a chronic condition can lead to emotional stress, and frequent seizures may impact mental health. Addressing these challenges is essential for holistic care.
Coping with Anxiety and Depression
Many people with epilepsy experience anxiety about when and where the next seizure might occur. Depression can also develop due to the social isolation or lifestyle limitations imposed by the condition. Regular therapy sessions with a psychologist or psychiatrist can help.
- Medication: Some individuals may benefit from antidepressants or anti-anxiety medication alongside their epilepsy treatment.
Social Stigma and Emotional Well-Being
People with epilepsy sometimes face stigma or discrimination due to misunderstandings about the condition. Fear of being judged can lead to isolation, affecting emotional health.
- Building Awareness: Educating friends, family, and colleagues about epilepsy can reduce stigma and foster support.
Support Groups and Counseling
Participating in epilepsy support groups helps individuals connect with others facing similar challenges. Sharing experiences and advice can ease emotional burdens and foster a sense of community.
10. Epilepsy in Children: Challenges and Solutions
Epilepsy presents unique challenges for children and their families, from managing seizures at school to ensuring normal development. However, with the right interventions, children with epilepsy can thrive academically and socially.
Recognizing Pediatric Seizures
Seizures in children can sometimes go unnoticed, especially if they appear as brief staring spells or subtle muscle twitches. Teachers and parents should be vigilant and track any unusual behavior, as early diagnosis can prevent complications.
School and Learning Accommodations
Children with epilepsy may need academic accommodations, such as extra time for exams or access to a quiet room in case of a seizure. Schools can implement Individualized Education Plans (IEPs) or 504 Plans to support learning.
- Teacher Training: Educating school staff on seizure management ensures children are safe and well-supported.
Parental Support and Guidance
Parents play a crucial role in managing their child’s epilepsy by keeping a seizure diary, ensuring medication compliance, and communicating with healthcare providers. Parenting a child with epilepsy can be stressful, so self-care for parents is also essential.
11. Epilepsy in Adults and Seniors: Special Considerations
Epilepsy can develop at any age, but managing it in adults and seniors presents unique challenges. Factors like aging, co-existing medical conditions, and lifestyle changes must be taken into account.
Aging with Epilepsy
For older adults, epilepsy can complicate other age-related conditions like memory loss or dementia. Doctors need to carefully manage medications to avoid interactions with treatments for high blood pressure, diabetes, or other chronic conditions.
Managing Epilepsy Alongside Other Health Conditions
Adults with epilepsy may have other health issues like heart disease or mental health conditions. Coordinating care between specialists ensures that treatments do not interfere with each other.
Driving and Independence Issues
Epilepsy can impact independence, especially if seizures are uncontrolled. Many regions have driving restrictions for individuals with epilepsy until they remain seizure-free for a specific period. Maintaining social and physical activity is essential to preserve quality of life, even with these restrictions.
12. Myths and Facts about Epilepsy
There are many myths and misconceptions about epilepsy that contribute to stigma and misinformation. Understanding the truth behind these myths is crucial for promoting awareness and acceptance.
Myth: Epilepsy Is Always Inherited
While genetics can play a role in some types of epilepsy, not everyone with the condition has a family history of it. Epilepsy can also result from brain injuries, infections, or developmental conditions.
Myth: Epilepsy Means You Cannot Live a Normal Life
With the right treatment, most people with epilepsy can live fulfilling lives, including working, driving, and pursuing hobbies. Medication, therapy, and lifestyle adjustments allow many to manage their seizures effectively.
Myth: Seizures Always Involve Convulsions
Not all seizures cause convulsions. Some involve brief lapses of consciousness, like absence seizures, where the person may appear to be staring into space. Recognizing the different types of seizures helps people respond appropriately to each situation.
13. Emergency Care for Seizures: What to Do
Knowing how to respond when someone has a seizure is crucial. Providing the right care can prevent injury and ensure the person’s safety during and after the episode.
First Aid Tips for Seizures
- Stay Calm: It’s essential to remain calm and reassure others around you.
- Time the Seizure: Track the duration to help medical professionals later.
- Protect from Injury: Clear the area of sharp objects, and gently turn the person on their side to prevent choking.
- Do Not Restrain: Never try to hold the person down or force anything into their mouth.
When to Call an Ambulance
- If the seizure lasts more than 5 minutes
- If the person has difficulty breathing or regaining consciousness
- If another seizure begins immediately after the first
- If the seizure happens in water or results in injury
Helping a Person Recover Safely
After the seizure ends, the person may feel disoriented or tired. Offer reassurance, stay with them until they are fully alert, and make them comfortable. If they do not recover quickly, seek medical help.
14. Future of Epilepsy Treatment: Ongoing Research and Advances
The landscape of epilepsy treatment is continuously evolving as researchers explore new ways to improve outcomes for patients. Several exciting advancements hold promise for the future.
New Medications and Therapies in Development
Researchers are working on next-generation anti-seizure medications with fewer side effects and improved effectiveness. These drugs aim to target the underlying causes of epilepsy rather than just managing symptoms.
The Role of AI and Personalized Medicine
Artificial intelligence (AI) is playing a growing role in epilepsy care. Machine learning algorithms can analyze seizure patterns to predict episodes, helping doctors personalize treatment plans. Personalized medicine based on genetic profiling is also opening new avenues for tailored therapies.
Ongoing Clinical Trials and Studies
Several clinical trials are underway to test new therapies, brain implants, and non-invasive devices. Ongoing studies on the impact of diet and lifestyle on seizure control could revolutionize how epilepsy is managed in the future.
15. When to See a Doctor?
- After a First-Time Seizure: Always consult a neurologist after the first episode.
- If Seizures Increase in Frequency: Frequent or severe seizures may indicate a need for medication adjustment.
- Impact on Daily Life or Mental Health: If seizures interfere with work, social life, or mental well-being, a doctor’s intervention is necessary.
- Seizure Lasts Over 5 Minutes: This is a medical emergency requiring immediate care.
16. Frequently Asked Questions (FAQs)
Q. What are the common triggers for epilepsy?
Ans. Common triggers include lack of sleep, stress, alcohol consumption, flashing lights, and skipping medication. Keeping a seizure diary helps identify personal triggers, allowing patients to minimize exposure and reduce episodes.
Q. Can stress cause seizures?
Ans. Yes, stress can act as a trigger for seizures, especially in individuals with epilepsy. Emotional stress can alter brain function and increase the risk of seizures. Managing stress through relaxation techniques and therapy is essential for seizure control.
Q. Is epilepsy curable?
Ans. Epilepsy is usually a lifelong condition, but it can be well-managed with medication and lifestyle changes. In some cases, especially in children, epilepsy can go into remission, meaning seizures stop for a prolonged period without medication. However, there is no universal cure.
Q. Are all seizures dangerous?
Ans. Not all seizures are dangerous, but they can lead to injury if they occur in unsafe situations (e.g., swimming or driving). Prolonged seizures (status epilepticus) are life-threatening and require immediate medical intervention.
Q. Can epilepsy affect mental health?
Ans. Yes, epilepsy can impact mental health, increasing the risk of anxiety, depression, and emotional stress. Managing epilepsy alongside mental health through therapy and counseling can significantly improve quality of life.
Conclusion: Managing Epilepsy for a Healthier Life
Found this helpful? Share this article with your friends and family!


3 thoughts on “Unlock Hope: Managing Epilepsy with Effective 16 Tips”