- 1. Introduction to GERD
- 2. Understanding GERD: The Problem
- 3. Agitating the Problem: How GERD Disrupts Life
- 4. Solution: Managing and Treating GERD
- 5. When to See a Doctor?
- 6. Diagnosis of GERD: What to Expect
- 7. Long-Term Risks of Untreated GERD
- 8. Preventing GERD Flare-Ups: What Works?
- 9. Myths about GERD: Debunking Misconceptions
- 10. Living with GERD: Realistic Tips for Daily Life
- 11. When GERD Becomes Chronic: What You Should Know
- 12. FAQs about GERD
1. Introduction to GERD
Gastroesophageal Reflux Disease, commonly known as GERD, is a chronic digestive disorder where stomach acid flows back into the oesophagus. This acid reflux can cause discomfort and disrupt daily activities. Many people experience occasional acid reflux, but when it occurs frequently, it may develop into GERD.
GERD affects millions of people worldwide, and it can interfere with work, sleep, and diet if not managed properly. Understanding the causes, symptoms, and available treatments is essential for maintaining long-term digestive health.
2. Understanding GERD: The Problem
When you eat, food passes through your oesophagus and enters the stomach. A muscle called the lower oesophageal sphincter (LES) opens to allow food to enter the stomach and closes to prevent acid from flowing back. In GERD, the LES becomes weak or relaxes when it shouldn’t, allowing stomach contents to move up into the oesophagus. This backward flow irritates the oesophagus, leading to uncomfortable symptoms like heartburn.
GERD is different from occasional heartburn. While most people experience mild acid reflux now and then, GERD involves chronic or severe symptoms that occur at least twice a week.
2.1 Causes of GERD
- Weak LES: When the lower oesophageal sphincter does not function properly, it allows acid to flow back.
- Obesity: Excess abdominal pressure can push stomach contents into the oesophagus.
- Pregnancy: Hormonal changes and pressure on the stomach during pregnancy increase the risk of GERD.
- Smoking and Alcohol: Both substances weaken the LES, contributing to reflux.
- Trigger Foods: Spicy, fatty, or acidic foods (like tomatoes and citrus) can worsen GERD symptoms.
3. Agitating the Problem: How GERD Disrupts Life
Living with GERD can be challenging. The burning sensation in the chest and frequent regurgitation of food often interfere with meals and sleep. Many people with GERD find it difficult to focus on work or enjoy social situations, knowing a flare-up could occur anytime. If left untreated, GERD can also lead to serious complications like esophagitis, ulcers, or even cancer.
Symptoms can vary in severity. For some, GERD causes mild discomfort, but for others, the symptoms may be so severe that they disrupt everyday life.
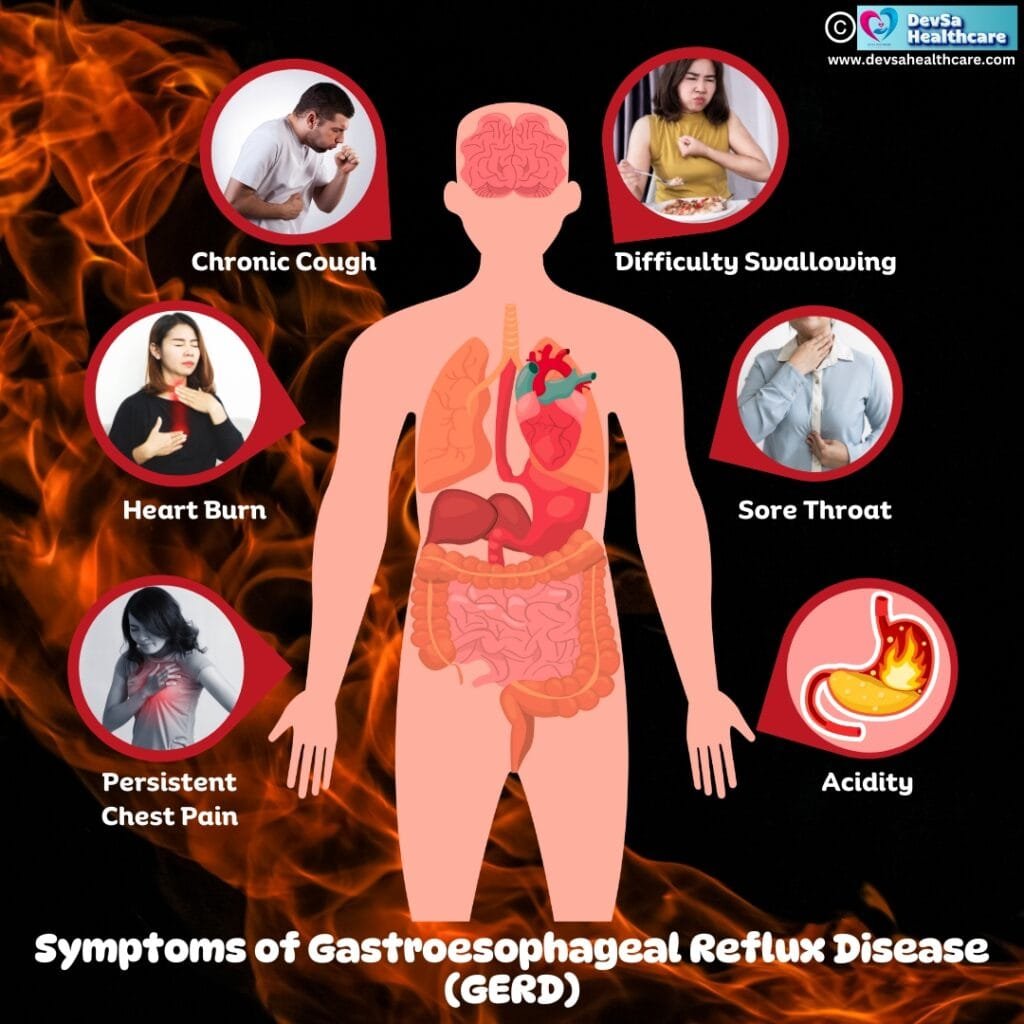
3.1 Common Symptoms of GERD
- Persistent Heartburn: A burning sensation in the chest, especially after eating.
- Regurgitation: Food or sour liquid returning to the mouth.
- Chest Pain: Sometimes mistaken for heart-related issues.
- Difficulty Swallowing: A sensation of food being stuck in the throat.
- Chronic Cough: Often due to irritation from acid in the throat or airways.
3.2 GERD in Children: Special Considerations
Children and infants may experience GERD differently. Infants often spit up frequently, but when it causes discomfort, refusal to eat, or weight loss, it may indicate GERD. Symptoms in older children may include persistent cough, wheezing, or difficulty swallowing. Early diagnosis and treatment are essential for proper development.
4. Solution: Managing and Treating GERD
GERD is manageable with the right combination of lifestyle changes and medical treatment. Addressing the underlying causes is crucial to finding relief. Not every case requires medication, and some people successfully manage symptoms with simple adjustments to diet and daily habits.
4.1 Lifestyle Changes for GERD
- Diet Modifications: Avoid foods that trigger symptoms, like fried foods, chocolate, and carbonated drinks.
- Weight Management: Losing even a small amount of weight can reduce pressure on the stomach.
- Quitting Smoking: This helps restore LES function and reduces acid reflux.
- Sleeping Position: Elevating the head of the bed can prevent nighttime reflux.
- Eating Habits: Eating smaller meals and avoiding meals right before bed can help.
4.2 Medical Treatments for GERD
- Antacids: These provide quick relief by neutralizing stomach acid.
- H2 Blockers: Reduce acid production to prevent symptoms.
- Proton Pump Inhibitors (PPIs): Stronger medication that blocks acid production and helps heal the oesophagus.
- Surgery: In severe cases, procedures like fundoplication are used to strengthen the LES and prevent reflux.
5. When to See a Doctor?
You should consult a doctor if lifestyle changes and over-the-counter medications don’t improve your symptoms. Persistent GERD may lead to complications if left untreated. Here are signs that require immediate medical attention:
- Severe Chest Pain: Especially if it mimics a heart attack.
- Difficulty Swallowing: This could indicate narrowing or damage to the oesophagus.
- Unexplained Weight Loss: GERD may be interfering with your ability to eat or digest food properly.
- Vomiting Blood or Black Stool: These may be signs of bleeding in the digestive tract.
- Chronic Hoarseness or Cough: These symptoms might indicate acid affecting the throat or airways.
Seeking early medical help ensures that any underlying issues are identified, and treatment can prevent complications such as Barrett’s oesophagus, a condition linked to oesophageal cancer.
6. Diagnosis of GERD: What to Expect
Diagnosing GERD requires a combination of your medical history, symptom patterns, and specific tests. Your doctor will start by asking about the frequency and severity of your heartburn, as well as any lifestyle factors or medications that might contribute.
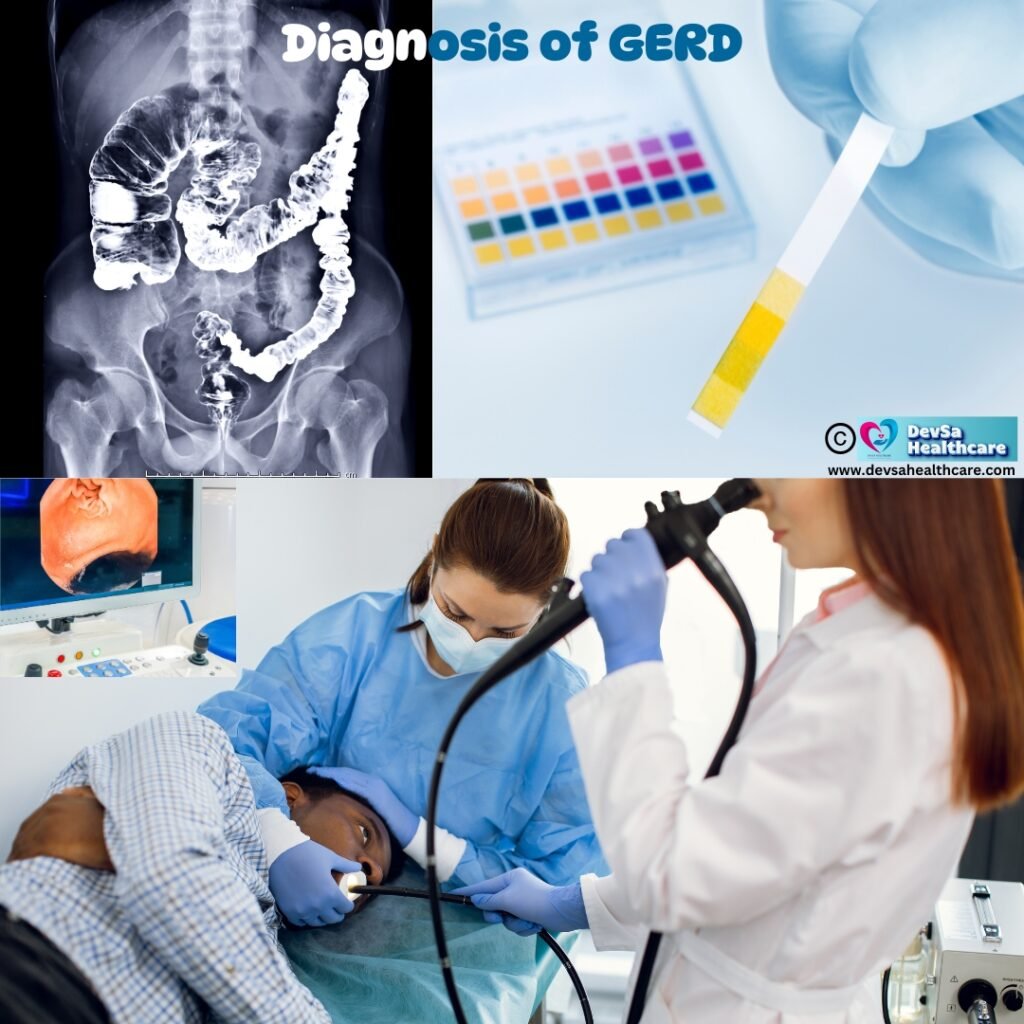
If the symptoms are persistent, further diagnostic tests may be required:
- Endoscopy: A thin, flexible tube with a camera is inserted into the oesophagus to look for inflammation, ulcers, or damage to the lining.
- pH Monitoring: This test measures the level of acidity in the oesophagus over 24 hours, helping to confirm reflux.
- Oesophageal Manometry: This measures the strength and coordination of the muscles in the oesophagus to see if the LES is functioning properly.
- Barium Swallow: An X-ray test used to spot structural issues, such as narrowing of the oesophagus.
These tests allow doctors to determine the severity of GERD and recommend the appropriate course of action.
7. Long-Term Risks of Untreated GERD
If GERD is not properly managed, it can lead to serious health complications over time. Acid exposure damages the Oesophageal lining, increasing the risk of inflammation and more severe issues.
- Esophagitis: Chronic acid reflux can cause inflammation, leading to pain and difficulty swallowing.
- Oesophageal Strictures: Over time, scarring can cause the oesophagus to narrow, making it hard to swallow food.
- Barrett’s Oesophagus: In some cases, cells in the oesophagus change due to long-term acid exposure, increasing the risk of Oesophageal cancer.
- Respiratory Issues: GERD can trigger asthma or worsen existing conditions by irritating the airways.
Monitoring and managing GERD is essential to avoid these long-term risks and maintain a healthy digestive system.
8. Preventing GERD Flare-Ups: What Works?
Prevention plays a key role in managing GERD. Making small but consistent changes to your lifestyle can greatly reduce the frequency of flare-ups.
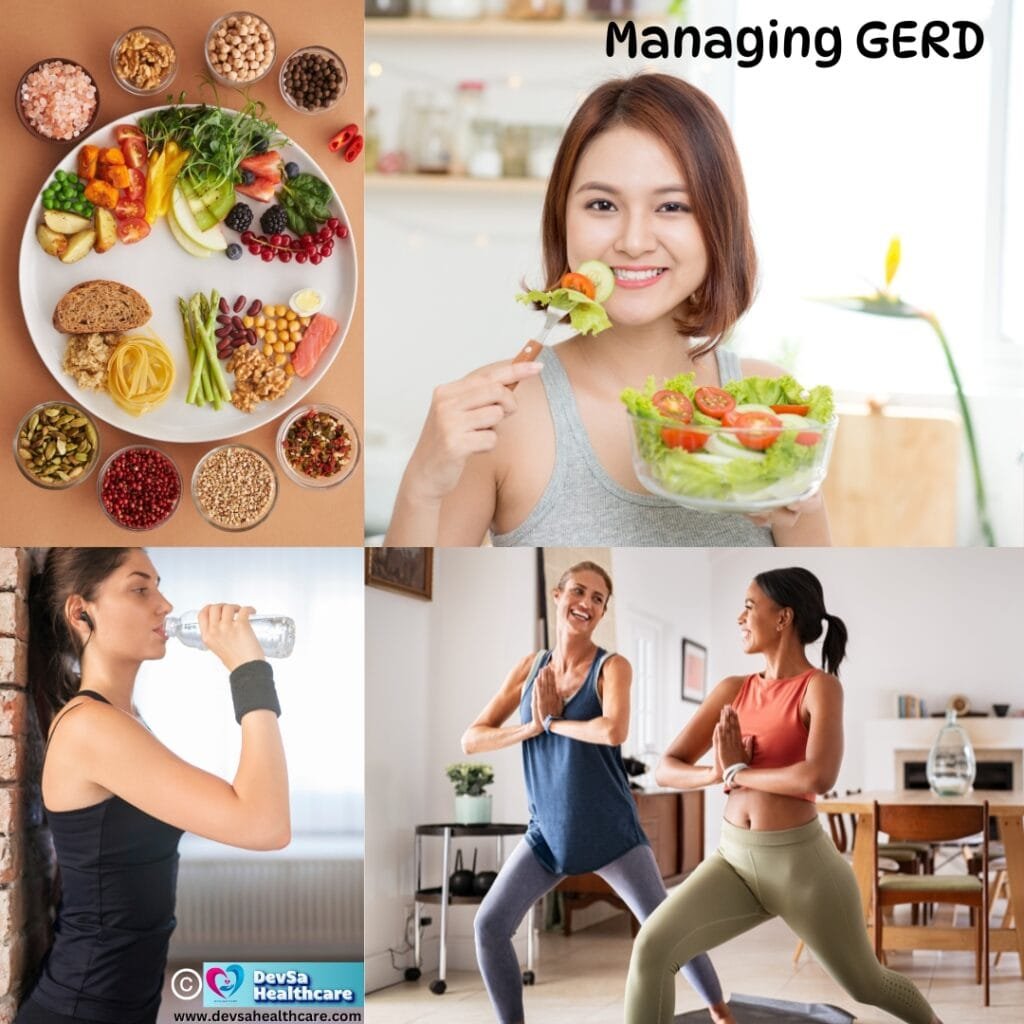
- Create a GERD-Friendly Meal Plan: Focus on foods that are less likely to trigger reflux, such as lean proteins, vegetables, and non-citrus fruits.
- Eat Smaller Portions: Large meals increase stomach pressure, which can push acid into the oesophagus.
- Stay Upright After Eating: Avoid lying down immediately after meals to reduce the risk of reflux.
- Elevate Your Head During Sleep: Use a wedge pillow or elevate the head of your bed to prevent nighttime reflux.
- Keep Track of Triggers: Use a food diary to identify specific foods that cause symptoms and adjust your diet accordingly.
Consistency is the key to preventing GERD symptoms from recurring.
9. Myths about GERD: Debunking Misconceptions
There are several common misconceptions about GERD, which can lead to confusion about how to manage the condition effectively. Let’s clear up a few myths:
- Myth: GERD is caused only by spicy food
Fact: While spicy food can trigger symptoms, other factors like stress, smoking, and overeating also play a significant role. - Myth: All chest pain is GERD-related
Fact: GERD can cause chest discomfort, but chest pain should never be ignored, as it could indicate heart issues. Seek medical advice if you’re unsure. - Myth: Once you take medication, GERD is cured forever
Fact: Medications can control symptoms, but lifestyle changes are necessary for long-term management. GERD often requires ongoing care.
Understanding these myths helps people set realistic expectations about treatment.
10. Living with GERD: Realistic Tips for Daily Life
Managing GERD long-term requires adjustments, but with the right approach, you can still enjoy life. Here are some practical tips for handling GERD:
- At Work: If GERD affects your focus, bring GERD-friendly snacks, and avoid large meals during work hours. Drinking water regularly can also help soothe the oesophagus.
- Social Events: When eating out, choose grilled or baked options over fried foods. It’s okay to politely decline certain foods that might trigger reflux.
- Travel Tips: Plan ahead by packing medications, antacids, and healthy snacks. Stay hydrated during travel and avoid heavy meals before long journeys.
- Physical Activity: Moderate exercise like walking or yoga can improve digestion and reduce reflux. Avoid vigorous activity immediately after eating.
- Positive Mindset: Accept that GERD may require ongoing attention. Focus on what you can control, like your diet and habits, instead of worrying about occasional flare-ups.
By making intentional choices, it’s possible to lead a full and active life with GERD.
11. When GERD Becomes Chronic: What You Should Know
For some individuals, GERD becomes a chronic condition that requires long-term management. Chronic GERD means that symptoms persist despite initial treatment or return frequently after periods of relief. This type of reflux may need continuous lifestyle adjustments and stronger medical intervention.
Managing chronic GERD often involves:
- Long-term medication use: Doctors may prescribe ongoing use of proton pump inhibitors (PPIs) to manage severe cases.
- Regular check-ups: Routine visits help monitor symptoms and catch complications early.
- Surgical intervention: If medications do not control symptoms, surgery like fundoplication might be necessary to tighten the LES.
- Dietary adjustments: Chronic GERD patients often need to avoid trigger foods indefinitely.
It is essential to treat chronic GERD proactively to avoid long-term complications and maintain a good quality of life.
12. FAQs about GERD
1. Can GERD be cured completely?
While some people find long-term relief through lifestyle changes and medication, GERD is a chronic condition for many. Management is key, but symptoms may still return occasionally.
2. What foods should I avoid if I have GERD?
It’s best to avoid fried foods, chocolate, caffeine, alcohol, citrus fruits, tomatoes, and carbonated drinks. Keeping a food diary can help identify individual triggers.
3. How is GERD different from heartburn?
Heartburn is a symptom—a burning sensation in the chest caused by acid reflux. GERD, on the other hand, is a chronic condition that involves frequent acid reflux episodes and additional symptoms like regurgitation and difficulty swallowing.
4. Can stress cause GERD symptoms?
Yes, stress can trigger or worsen GERD symptoms. Stress affects digestion and can lead to behaviours like overeating, which increases reflux.
5. Is surgery necessary for severe GERD cases?
Surgery is not the first option. It is usually recommended only when lifestyle changes and medications fail to manage symptoms. Fundoplication and other procedures aim to strengthen the LES to prevent reflux.
Conclusion: Managing Epilepsy for a Healthier Life
Found this helpful? Share this article with your friends and family!

2 thoughts on “Ultimate Guide to GERD Relief: Say Goodbye to Heartburn”